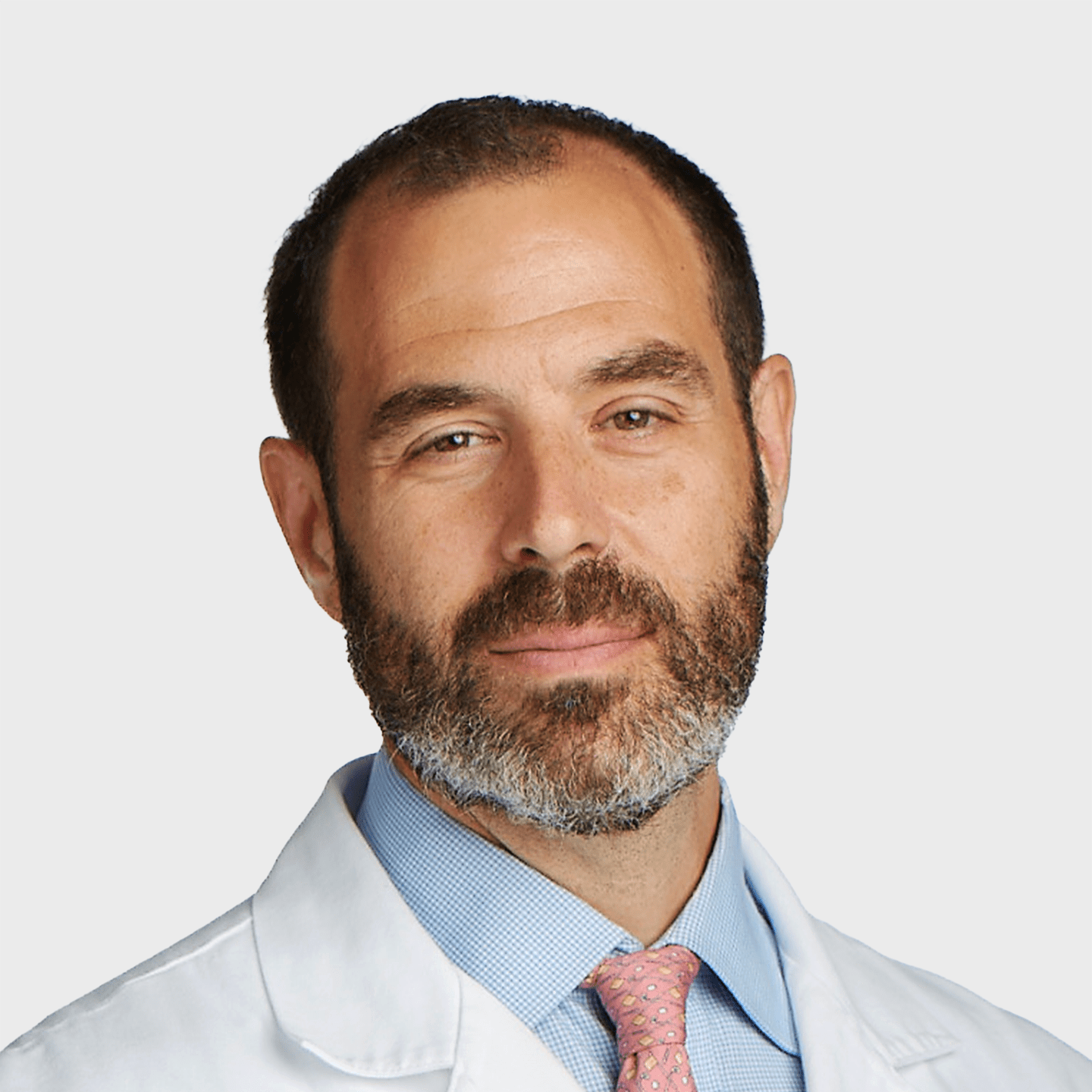

Scott L. Simon, MD
Clinical Interests
Spondylolisthesis, Degenerative Disc Disease, Pinched Nerves, Herniated/Bulging Disc Treatments, Fusion Sparing Surgery, Anterior Cervical Discectomy & Fusion, Cervical Foraminotomy
Located In
Stamford
- ql-locations, ql-background, ql-reviews
About
Scott Simon, MD is a neurosurgeon who specializes in the treatment of spinal disorders including operative and non-operative treatment of spine deformity and scoliosis. He is one of just a few physicians nationwide trained in neurological surgery and orthopedic techniques to treat scoliosis in adolescents and adults. Dr. Simon has extensive experience in minimally invasive spine surgery and was the first surgeon in the region to perform spine surgery using the highly advanced robotic navigation system, Globus Excelsius, GP.
His clinical interests encompass a range of advanced techniques and conditions such as fusionless options for spondylolisthesis, degenerative disc disease, pinched nerves, herniated/bulging disc treatments, fusion sparing surgery, minimally invasive lumbar discectomy, anterior cervical discectomy and fusion, robot-assisted spinal fusion and cervical foraminotomy.
Dr. Simon is affiliated with Greenwich and Stamford Hospitals. He graduated from medical school at UMDNJ – New Jersey Medical School, now known as Rutgers Medical School. Dr. Simon then completed his residency at The University of Pennsylvania Department of Neurosurgery, and his fellowship training in Spine Surgery and Scoliosis at The Shriners Hospital for Children in Philadelphia.
Aetna
- Commercial Plans (Including APCN Plus, We do not accept regular APCN)
- Managed Medicare
Anthem Blue Cross Blue Shield of CT
- Commercial and Exchange
- Managed Medicare
Blue Cross Blue Shield (Plans Outside CT)
- Cards with the “PPO” inside the suitcase logo
CarePartners of Connecticut
- Managed Medicare (HMO/PPO)
Cigna
- Commercial, MetroNY, and LocalPlus
- Cigna+Oscar, Cigna+MVP (CT Locations Only)
ConnectiCare
- Commercial and Exchange (Except “Value” Network)
- Managed Medicare
Connecticut Medicaid
Connecticut State Workers’ Compensation
EmblemHealth
- Emblem Commercial and Exchange (Except for Millennium and Enhanced Care Prime Networks)
- Managed Medicare (VIP Prime, Bold, Reserve)
Harvard Pilgrim
- Through United Shared Services – ONS Harrison location only.
Medicare (Including Railroad Medicare)
Oxford
- Liberty and Freedom Plans
UHC/NYSHIP/NY Government Empire Plan
United Healthcare
- All Commercial Plans (Except Indemnity and Compass)
- Managed Medicare
Orthopaedic & Neurosurgery Specialists (ONS) accepts most major insurance plans. Please see the list of accepted insurance plans above and confirm that ONS participates with your plan prior to scheduling an appointment. Certain insurance plans are limited to specific regions and physicians. If you have additional questions, please call our offices at (203) 869-1145 ext. 279 and our team will be happy to provide additional information.
Locations
Fellowship
Fellowship in Spinal Surgery and Deformity: Shriners Hospital for Children, Philadelphia Unit, Philadelphia, PA
Medical School
Rutgers Medical School, Newark, NJ
Residency
Department of Neurosurgery, The University of Pennsylvania, Philadelphia, PA
College
Emory University, Atlanta, GA
- The American Board of Neurological Surgery: Neurological Surgery Board Certification
Memberships
- American Association of Neurological Surgeons (AANS)
- American Board of Neurological Surgery (ABNS)
- Congress of Neurological Surgeons
- Joint Section on Disorders of the Spine and Peripheral Nerves
- Stamford Hospital ICU Committee
- Stamford Hospital OR Committee
- Stamford Hospital Peer Review Committee
- The Association for Ethics in Spine Surgery
- The Cyberknife Society
Appointments
- Shriners Hospital for Children, Philadelphia, PA. Consultant
- Former Stamford Hospital Neurosurgical Director of Cyberknife Radiosurgery
- Former Stamford Hospital Neurosurgical Trauma Director
- Castle Connolly Top Doctors, 2012–Present
- Castle Connolly New York Metro Area Top Doctor, 2012–Present
- Connecticut Magazine Top Doctor 2011-2012, 2016, 2017, 2020-Present
- Greenwich Magazine Top Doctor in Fairfield County, 2012–Present
- New Canaan/Darien Magazine Top Doctor in Fairfield County, 2012–Present
- Stamford Magazine Top Doctor in Fairfield County, 2012-Present
- Westport Magazine Top Doctor in Fairfield County, 2012–Present
- New York Magazine Best Doctors, 2013–2020
- Fairfield Magazine Top Doctor, 2012–2017
- Simon SL, Marcotte P, Grady MS: Surgical Approaches and Techniques of Fixation of the Cervicothoracic Junction, in Dickman, Fehlings, Golaskan (eds): Spinal Cord and Spinal Column Tumors: Principles and Practice. New York, Theme, 2006.
- Simon SL, Schuster JM: Posterior Thoracic Instrumentation, in Youman’s (eds): Neurological Surgery, 5th Edition. Philadelphia, W.B. Saunders Co., 2003.
- Simon SL, Auerbach JD, Garg S, Sutton LN, Telfeian AE, Dormans JP. Efficacy of spinal instrumentation and fusion in the prevention of postlaminectomy spinal deformity in children with intramedullary spinal cord tumors. J Pediatr Orthop. 2008 Mar;28(2):244-9. PMID: 18388723 [PubMed – in process]
- Simon SL, Betz RR: Spinal Cord Injury in Children Evaluation and Early Treatment Principles, in Kim, Betz (eds): Surgery of the Pediatric Spine. New York, Thieme, 2007.
- Simon SL, D’Andrea L, Clements D, Betz RR. Evoked and spontaneous electromyography to evaluate upper thoracic pedicle screw placement. (In preparation).
- Simon SL, Garg S, Burnett MG, Telfeian A, Dormans J, Sutton LN. The efficacy of prophylactic spinal fusion in the prevention of post-surgical spinal deformity in pediatric spinal cord tumors. (Spine- in revision).
- Chen HI, Heuer GG, Zaghloul K, Simon SL, Weigele JB, Grady MS. Lumbar vertebral hemangioma presenting with the acute onset of neurological symptoms. Case report. J Neurosurg Spine. 2007 Jul;7(1):80-5.
- Whitmore RG, Simon SL, Hurst RW, Nisenbaum HL, Kasner SE, Zager EL. Bow hunter’s syndrome caused by accessory cervical ossification: posterolateral decompression and the use of intraoperative Doppler ultrasonography. Surg Neurol. 2007 Feb;67(2):169-71. Epub 2006 Nov 3.
- Simon S, Davis M, Odhner D, Udupa J, Winkelstein B. CT imaging techniques for describing motions of the cervicothoracic junction and cervical spine during flexion, extension, and cervical traction. Spine. 2006 Jan 1;31(1):44-50.
- Simon SL, Douglas P, Baltuch GH Jaggi JL. Error Analysis of MRI and Leskell Stereotactic Frame Target Localization in Deep Brain Stimulation Surgery. Stereotact Funct Neurosurg. 2005 Feb 4;83(1):1-5.
- Jiamin Liu, Jayaram K Udupa, Punam K Saha, Dewey Odhner, Bruce E. Hirsch, Sorin Siegler, Scott Simon, Beth A. Winkelstein. Rigid Model-based 3D segmentation of the bones of joints in MR and CT image. SPIE Medical Imaging Conference, 2005.
- Simon SL, Moonis G, Judkins AR, Scobie J, Burnett MG, Riina HA, Judy KD. Intracranial capillary hemangioma: case report and review of the literature. Surg Neurol. 2005 Aug;64(2):154-9.
- Kreiger PA, Okada Y, Simon S, Rorke LB, Louis DN, Golden, JA. Losses of chromosomes 1p and 19q are rare in pediatric oligodendrogliomas. Acta Neuropathologica. Acta Neuropathol (Berl). 2005 Mar 1.
- Simon SL, Pahl MA, Marcotte PJ, Vaccaro AR, Grady MS: The management of infections involving the cervicothoracic junction. Seminars in Spine Surgery 2004 Sep;16(3):206-213.
- Huang JH, Simon SL, Nagpal S, Nelson PT, Zager EL. Management of patients with schwannomatosis: Report of six cases and review of the literature. Surg Neurol. 2004 Oct;62(4):353-61.
- Moonis G, Hurst RW, Simon SL, Zager EL. Intradural venous varix: a rare cause of an intradural lumbar spine lesion. Spine. 2003 Oct 15;28(20):E430-2.
- Simon SL, Telfeian A, Duhaime AC. Complications of Invasive Monitoring Used in Intractable Pediatric Epilepsy. Pediatric Neurosurgery2003 Jan;38(1):47-52.
- Moonis G, Granados A, Simon SL. Epidural hematoma as a complication of sphenoid sinusitis and epidural abscess. A case report and literature review. Clinical Imaging 2002 Nov-Dec;26(6):382-5.
- Telfeian AE, Berqvist C, Danielak C, Simon SL, Duhaime AC. Recovery of language after hemispherectomy in a sixteen-year-old girl with late onset seizures. Pediatric Neurosurgery 2002 July;37(1):19-21.
- Simon SL, Abrahams JM, Rushton S, Grady MS. Case Report: Intramedulary injection of contast into the cervical spinal cord. Spine2002;27(10):E274-277.
- Schulman BJ, Loevner LA, Simon S. Imaging Corner: Vertebral osteonecrosis. Spine 2000;25(18):2419-2420.
- Phillips VL, Potter SJ, Simon SL. Special care units for Alzheimer’s patients: their role in the nursing home market. J Health Hum Serv Adm 1998; 20(3):300-310