ONS Blog
 Orthopaedic & Neurosurgery Specialists Expands Physical and Occupational Therapy Clinic in Wilton, CT
Orthopaedic & Neurosurgery Specialists Expands Physical and Occupational Therapy Clinic in Wilton, CT 
 Sports MedicineAn Active Mom’s Return from ACL Surgery
Sports MedicineAn Active Mom’s Return from ACL Surgery

 Foot and AnkleUnderstanding Achilles Tendon Injuries: Causes, Treatment, and Recovery
Foot and AnkleUnderstanding Achilles Tendon Injuries: Causes, Treatment, and Recovery


 Distance Runner Reclaims His Stride Thanks to Dr. Sethi and ONS
Distance Runner Reclaims His Stride Thanks to Dr. Sethi and ONS
A severe knee injury couldn’t stop Kyle Zilles—thanks to Dr. Sethi and ONS

 What to Know About Minimally Invasive Achilles Tendon Surgery
What to Know About Minimally Invasive Achilles Tendon Surgery

 Foot and AnkleBunion Q&A: What to Know About Symptoms, Treatment Options, and Recovery from Foot & Ankle Experts at ONS
Foot and AnkleBunion Q&A: What to Know About Symptoms, Treatment Options, and Recovery from Foot & Ankle Experts at ONS


 Foot and AnkleAnkle Sprains, Fractures, and Instability: A Q&A with Foot & Ankle Experts at ONS
Foot and AnkleAnkle Sprains, Fractures, and Instability: A Q&A with Foot & Ankle Experts at ONS


 Sports MedicineRotator Cuff Injury Prevention in Spring Sports
Sports MedicineRotator Cuff Injury Prevention in Spring Sports

 U.S. News & World Report Names The Stamford Ambulatory Surgical Center Best Ambulatory Surgery Center For Second Straight Year
U.S. News & World Report Names The Stamford Ambulatory Surgical Center Best Ambulatory Surgery Center For Second Straight Year
 Sports MedicineIronman Competitor Back to Triathlons After Leg Surgery
Sports MedicineIronman Competitor Back to Triathlons After Leg Surgery

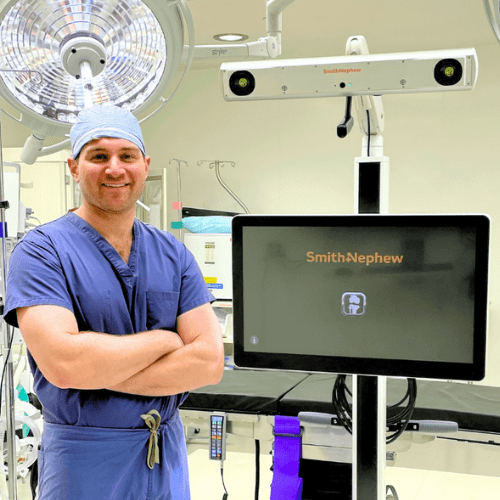 Hip and Knee ReplacementONS’ Stamford ASC Adds State-of-the-Art CORI Surgical System for Joint Replacement
Hip and Knee ReplacementONS’ Stamford ASC Adds State-of-the-Art CORI Surgical System for Joint Replacement

 Premier Lacrosse League Announces Partnership with Spire Orthopedic Partners as Exclusive Orthopedic & Physical Therapy Provider
Premier Lacrosse League Announces Partnership with Spire Orthopedic Partners as Exclusive Orthopedic & Physical Therapy Provider
 31 ONS Physicians Honored on the Castle Connolly 2025 Top Doctors and Rising Stars List
31 ONS Physicians Honored on the Castle Connolly 2025 Top Doctors and Rising Stars List
 PhysiatryShockwave Therapy for Orthopedic Conditions
PhysiatryShockwave Therapy for Orthopedic Conditions
Shockwave therapy is revolutionizing treatment for orthopedic conditions

 Sports MedicineHow Knee Surgery Helped Elizabeth Return to the Outdoors
Sports MedicineHow Knee Surgery Helped Elizabeth Return to the Outdoors

 Outpatient Joint ReplacementHow Are So Many Total Joint Replacements Performed in an Outpatient Setting?
Outpatient Joint ReplacementHow Are So Many Total Joint Replacements Performed in an Outpatient Setting?
Recent advancements have made outpatient surgery safe and effective.


 Sports MedicineKey Takeaways from Dr. Kowalsky's 2024 USA Rugby Tour Experience
Sports MedicineKey Takeaways from Dr. Kowalsky's 2024 USA Rugby Tour Experience

 Physician Spotlight on Dr. Michael B. Held
Physician Spotlight on Dr. Michael B. Held
Get to know Dr. Michael Held, hip and knee replacement surgeon at ONS!

 Sports MedicineAll About Pickleball: Injury Prevention Tips
Sports MedicineAll About Pickleball: Injury Prevention Tips

 Hand and Upper ExtremityWith expert care, a severe fracture is just a quick break from Kevin’s active lifestyle.
Hand and Upper ExtremityWith expert care, a severe fracture is just a quick break from Kevin’s active lifestyle.
Kevin gets back to the slopes thanks to Dr. Wei and ONS

 Sports MedicineBack on the Slopes: A Patient’s Return to Outdoor Activities After a Meniscus Tear
Sports MedicineBack on the Slopes: A Patient’s Return to Outdoor Activities After a Meniscus Tear

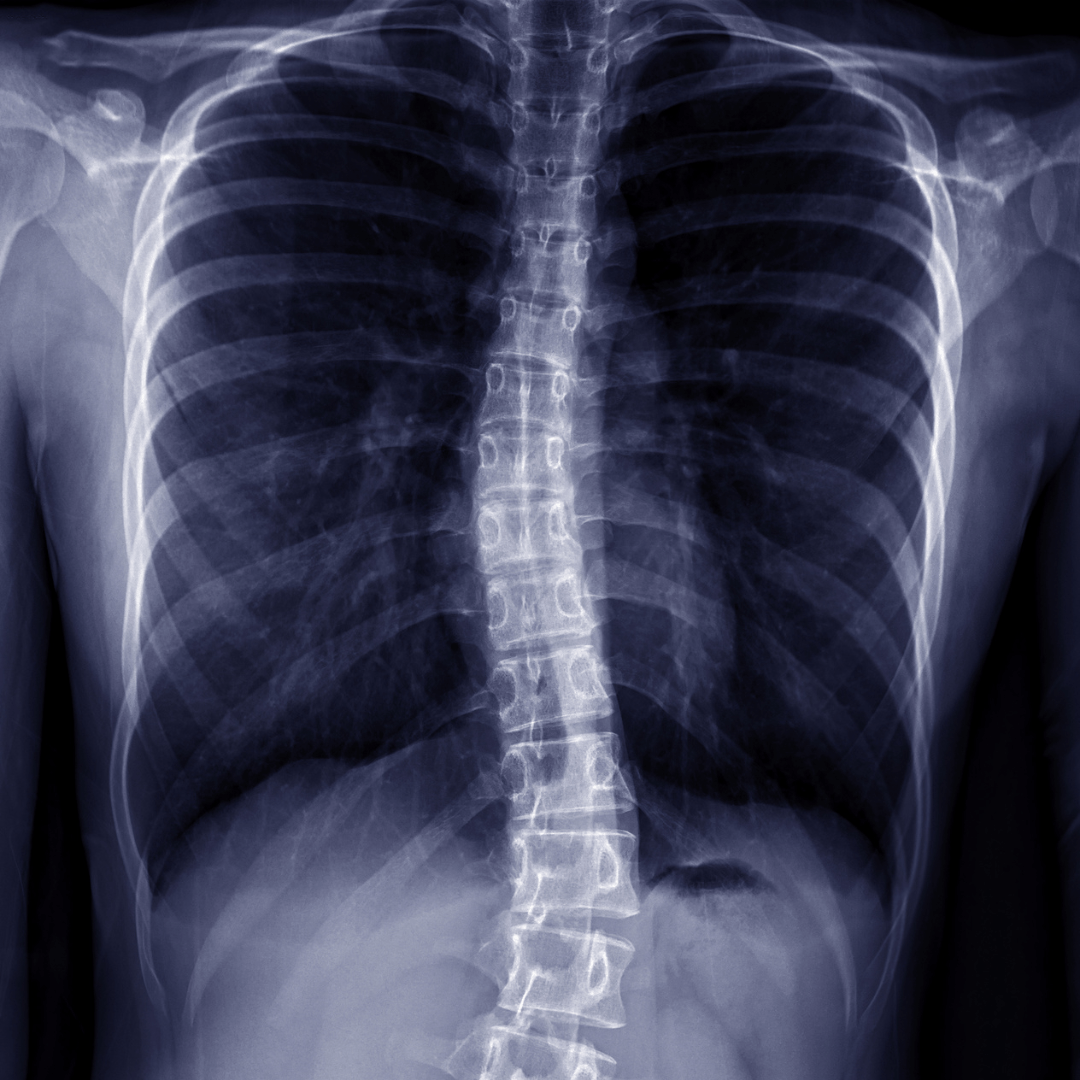 SpineUnderstanding Scoliosis
SpineUnderstanding Scoliosis

 Hand and Upper ExtremityA Journey to Recovery: How Dr. Vitale Restored Katherine’s Hand Function and Relieved Her Pain
Hand and Upper ExtremityA Journey to Recovery: How Dr. Vitale Restored Katherine’s Hand Function and Relieved Her Pain

 Sports MedicineAn ACL Recovery Story: Using Physical Therapy and Mini-Milestones
Sports MedicineAn ACL Recovery Story: Using Physical Therapy and Mini-Milestones

 U.S. News & World Report Names The Stamford Ambulatory Surgical Center Among Inaugural Edition of Best Ambulatory Surgery Centers in Connecticut
U.S. News & World Report Names The Stamford Ambulatory Surgical Center Among Inaugural Edition of Best Ambulatory Surgery Centers in Connecticut
Stamford ASC has been recognized as a Best ASC- Orthopedics & Spine 2024
 Hand and Upper ExtremityBouncing Back with ONS: A Young Gymnast's Triumph After a Broken Arm
Hand and Upper ExtremityBouncing Back with ONS: A Young Gymnast's Triumph After a Broken Arm
Young gymnast with injured arm wins big with Dr. Wei and ONS

 Rotator Cuff TearAvid Tennis Player Back in the Game through ONS
Rotator Cuff TearAvid Tennis Player Back in the Game through ONS
Scott found pain relief and is back to his active life through ONS

 SpineCatwalks and Courage: A Model Turned Military Member’s Path to Pain Relief
SpineCatwalks and Courage: A Model Turned Military Member’s Path to Pain Relief
 NeurosurgeryManaging a Chronic Neurological Condition with ONS Neurosurgeon
NeurosurgeryManaging a Chronic Neurological Condition with ONS Neurosurgeon

 Physician Spotlight on Dr. Eliana Cardozo
Physician Spotlight on Dr. Eliana Cardozo

 Physician Spotlight on Dr. Marc Otten
Physician Spotlight on Dr. Marc Otten

 Physician Spotlight on Dr. Frank Aversano
Physician Spotlight on Dr. Frank Aversano

 Physician Spotlight on Dr. Robert Merrill
Physician Spotlight on Dr. Robert Merrill

 Physician Spotlight on Dr. Jordan Pasternack
Physician Spotlight on Dr. Jordan Pasternack

 Orthopaedic & Neurosurgery Specialists Leads Connecticut Orthopedic Practices with 33 Castle Connolly 2024 Top Doctors and Rising Stars
Orthopaedic & Neurosurgery Specialists Leads Connecticut Orthopedic Practices with 33 Castle Connolly 2024 Top Doctors and Rising Stars
 Youth Sports Injury Prevention Virtual Event with House of Sports
Youth Sports Injury Prevention Virtual Event with House of Sports


 Hand and Upper ExtremityFrom Wrist to Heart: How a Hand and Upper Extremity Surgeon Changed My Life
Hand and Upper ExtremityFrom Wrist to Heart: How a Hand and Upper Extremity Surgeon Changed My Life
Ariff found relief for wrist pain and much more through Dr. Vitale and ONS

 Anterior Cruciate Ligament (ACL) ReconstructionBack in the Swing of Things: The Inspiring ACL Recovery Journey of a Champion College Softball Player
Anterior Cruciate Ligament (ACL) ReconstructionBack in the Swing of Things: The Inspiring ACL Recovery Journey of a Champion College Softball Player

 Sports MedicineThe Female Athlete in Her 40s and Beyond: How to Stay Healthy Virtual Seminar
Sports MedicineThe Female Athlete in Her 40s and Beyond: How to Stay Healthy Virtual Seminar

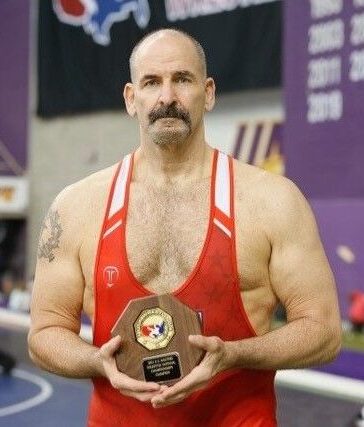 SpineBack on the Mat: A Wrestler’s Journey After Spine Surgery
SpineBack on the Mat: A Wrestler’s Journey After Spine Surgery
Lifelong wrestler makes his way back onto the mat with Dr. Simon and ONS
 Hip Replacement SurgeryA Patient’s Return to Competitive Dancing After Hip Replacement
Hip Replacement SurgeryA Patient’s Return to Competitive Dancing After Hip Replacement
Competitive dancer back on the floor thanks to Dr. Kevin Choo and ONS

 From Sidelines to State Championships: A High School Athlete’s ACL Recovery Story
From Sidelines to State Championships: A High School Athlete’s ACL Recovery Story

 Back for Another Round: A PGA Golfer’s Recovery Story
Back for Another Round: A PGA Golfer’s Recovery Story
PGA Professional Back on the Course with ONS After Hamstring Tear

 Sports MedicineFootball Injury Prevention Tips for High School Athletes
Sports MedicineFootball Injury Prevention Tips for High School Athletes

 Foot and AnkleONS Physician Spotlight on Foot & Ankle Specialist Andrew Pao, MD
Foot and AnkleONS Physician Spotlight on Foot & Ankle Specialist Andrew Pao, MD

 ONS Physician Spotlight on Rheumatologist Dr. Melissa LaRusso
ONS Physician Spotlight on Rheumatologist Dr. Melissa LaRusso


